When we think about strong teeth and healthy gums, minerals like calcium and fluoride often steal the spotlight. We focus on brushing away bacteria and avoiding sugar. But lurking beneath the surface, performing vital structural and supportive roles, is a crucial protein that’s fundamental to nearly every aspect of our oral health: collagen. Often associated with skin elasticity and joint health, collagen is, in fact, the most abundant protein in the human body, and its presence and integrity within our mouths are absolutely essential for maintaining resilient gums, anchoring teeth firmly in place, and even contributing to the structure of the teeth themselves.
Ignoring the health of our collagen matrix can have profound consequences for our oral well-being. From providing the firm yet flexible framework of our gums to forming the critical ligaments that hold teeth in their sockets, collagen is the unsung hero working tirelessly behind the scenes. Understanding its diverse functions within the oral cavity highlights the importance of lifestyle choices and professional care that support its production and preservation. Let’s explore the science behind this vital protein and its indispensable role in keeping our smiles healthy and strong.
Don't Delay Your Treatment
Let's create your personalised treatment plan right away with a complimentary consultation with our specialist dentists.
What Exactly is Collagen? The Body’s Scaffolding
Collagen isn’t a single substance but rather a family of proteins that act as the primary structural component of various connective tissues throughout the body – including skin, bones, tendons, ligaments, cartilage, and, importantly for us, gums and the structures supporting our teeth. Think of it as the body’s natural scaffolding or glue (‘kola’ is Greek for glue).
Its unique structure, typically a triple helix of amino acid chains, gives collagen remarkable tensile strength (resistance to pulling forces) combined with flexibility. There are many different types of collagen (at least 28 identified!), each adapted for specific functions. In the oral cavity, Type I collagen is particularly dominant, making up a significant portion of our gums, periodontal ligament, dentin, and the organic matrix of alveolar bone (the jawbone socket).
Our bodies continuously synthesize collagen, but this process requires specific building blocks (amino acids like glycine, proline, hydroxyproline) and essential co-factors, most notably Vitamin C. Factors like age, diet, lifestyle habits, and certain diseases can significantly impact both the production and breakdown of this vital protein.
Collagen: The Backbone of Healthy Gums (Gingiva)
Healthy gums are firm, resilient, and form a tight seal around the teeth, acting as a crucial barrier against bacterial invasion. Collagen is the star player in achieving this:
- Structural Integrity and Firmness: The dense network of Type I collagen fibers within the gum connective tissue (lamina propria) provides the tissue with its structure, shape, and resistance to the mechanical stresses of chewing. Healthy collagen levels contribute to that firm, stippled appearance often associated with healthy gingiva.
- Barrier Function: This collagen-rich matrix helps maintain the integrity of the gum tissue, preventing bacteria and their toxins from easily penetrating deeper tissues and entering the bloodstream.
- Wound Healing: Collagen synthesis is fundamental to tissue repair. Whenever there’s an injury to the gums – from minor cuts, vigorous brushing, dental procedures, or even infections – the body ramps up collagen production to form new tissue, close the wound, and restore structural integrity. Impaired collagen production significantly delays healing.
- Fighting Gum Disease: Ironically, while essential for health, collagen becomes a target during gum disease. The inflammation triggered by bacterial plaque releases enzymes (like collagenases) that actively break down collagen fibers in the gums. This destruction leads to the characteristic symptoms of periodontal gum diseases, such as loss of firmness, swelling, pocket formation, and gum recession. Maintaining healthy collagen is therefore crucial for *resisting* the progression of gum disease.
Without sufficient, healthy collagen, gums become weaker, more prone to bleeding and infection, and less effective as a protective barrier.
Don't Delay Your Treatment
Let's create your personalised treatment plan right away with a complimentary consultation with our specialist dentists.

Anchoring Our Teeth: Collagen in the Periodontal Ligament and Bone
Collagen’s role extends beyond the visible gum tissue to the critical structures that anchor teeth within the jaw:
1. The Periodontal Ligament (PDL)
This is a specialized connective tissue ligament that surrounds the tooth root and connects it to the alveolar bone socket. It’s composed primarily of densely packed Type I collagen fiber bundles (called Sharpey’s fibers where they insert into bone and cementum). The PDL serves several vital functions, all dependent on its collagen structure:
- Anchorage: It physically holds the tooth in its socket.
- Shock Absorption: The arrangement of collagen fibers allows for slight tooth movement during chewing, absorbing and distributing biting forces to prevent damage to the tooth and bone.
- Sensory Function: Contains nerve endings that provide feedback on pressure and pain.
- Formative/Nutritive: Contains cells that help maintain and repair the adjacent bone and cementum (the layer covering the root).
Breakdown of PDL collagen fibers due to advanced periodontitis is what leads to tooth mobility (loosening) and eventual tooth loss.
2. Alveolar Bone
While bone is mostly mineral, about 30% of its dry weight is an organic matrix, and roughly 90% of that organic matrix is Type I collagen. This collagen framework provides flexibility to the bone (preventing it from being too brittle) and acts as the scaffold upon which bone mineral crystals (hydroxyapatite) are deposited. Healthy bone turnover, essential for maintaining the integrity of tooth sockets, relies on this collagen matrix.
Beneath the Surface: Collagen Within the Tooth Structure (Dentin)
While enamel is almost entirely mineral, the underlying dentin – which makes up the bulk of the tooth – has a significant organic component. Approximately 20% of dentin by weight is organic matrix, and again, Type I collagen makes up about 90% of this matrix.
Don't Delay Your Treatment
Let's create your personalised treatment plan right away with a complimentary consultation with our specialist dentists.
In dentin, the collagen network forms an intricate scaffold that becomes mineralized with hydroxyapatite crystals. This collagen framework is crucial for:
- Providing Dentin Structure: It gives dentin some flexibility, making the tooth less brittle than if it were purely mineral.
- Guiding Mineralization: It directs the organized deposition of mineral crystals during tooth development.
- Supporting Enamel: Dentin provides the foundation upon which the harder enamel layer rests.
Damage to the dentinal collagen matrix (e.g., from deep decay or aggressive dental procedures) can compromise the tooth’s overall structural integrity.
Factors Influencing Collagen Health in Your Mouth
The status of collagen in your oral tissues isn’t static. Several factors influence its synthesis, maintenance, and degradation:
- Age: Natural collagen production tends to slow down as we age, which can contribute to thinner gums and slower healing.
- Vitamin C Deficiency: Vitamin C is an essential co-factor for enzymes involved in collagen synthesis and cross-linking. Severe deficiency (scurvy) famously leads to weakened collagen, resulting in bleeding gums, loosening teeth, and poor wound healing. Even subclinical deficiency can impair optimal collagen health.
- Dietary Protein/Amino Acids: Collagen is a protein, so adequate intake of protein, providing essential amino acids like proline and glycine, is necessary for its production. Copper and zinc are also important micronutrients.
- Smoking: Tobacco smoke contains numerous toxins that impair collagen synthesis, increase its breakdown, reduce blood flow (hindering nutrient delivery and healing), and significantly worsen gum disease.
- Gum Disease (Inflammation): As mentioned, the chronic inflammation in gingivitis and periodontitis leads to enzymatic destruction of collagen in the gums and PDL.
- Diabetes: Poorly controlled diabetes can impair collagen synthesis and cross-linking and slow down wound healing.
- Hormonal Changes: Fluctuations during pregnancy or menopause can sometimes affect gum tissue health, partly related to vascular and connective tissue changes.
- Genetic Factors: Certain rare genetic disorders directly affect collagen structure or production.
- Stress: Chronic stress leading to elevated cortisol levels might negatively impact collagen synthesis and wound healing.

Nourishing Your Network: Supporting Collagen for Optimal Oral Health
While we can’t stop aging, we can take proactive steps to support our body’s collagen production and protect the existing collagen network in our mouths:
- Eat a Collagen-Supportive Diet:
- Prioritize Vitamin C: Consume plenty of citrus fruits, berries, bell peppers, kiwi, broccoli, and leafy greens.
- Ensure Adequate Protein Intake: Include lean meats, poultry, fish, eggs, legumes, and dairy to provide necessary amino acids.
- Consider Bone Broth: While direct evidence for oral health benefits is limited, bone broth is rich in collagen components and minerals.
- Include Copper and Zinc Sources: Found in nuts, seeds, whole grains, shellfish, and beans.
- Maintain Excellent Oral Hygiene: This is non-negotiable for preventing gum disease, which directly destroys collagen. Brush thoroughly twice daily, floss daily, and consider an antiseptic mouthwash if recommended.
- Don’t Smoke or Use Tobacco: Quitting is one of the single best things you can do for your collagen health and overall oral wellness.
- Manage Systemic Conditions: Keep conditions like diabetes under good control through collaboration with your physician.
- Stay Hydrated: Water is essential for all bodily processes, including tissue health and saliva production.
- Regular Professional Dental Care:
- Routine check-ups and cleanings allow for early detection and management of gum disease. Comprehensive care under general dentistry is fundamental.
- Professional treatments for gum disease aim to halt the inflammatory process that destroys collagen.
- Ensuring adequate gum and bone health is vital before procedures like placing dental implants, which rely on a stable collagen-rich foundation.
- Healing after surgical interventions in the mouth is heavily dependent on robust collagen synthesis.
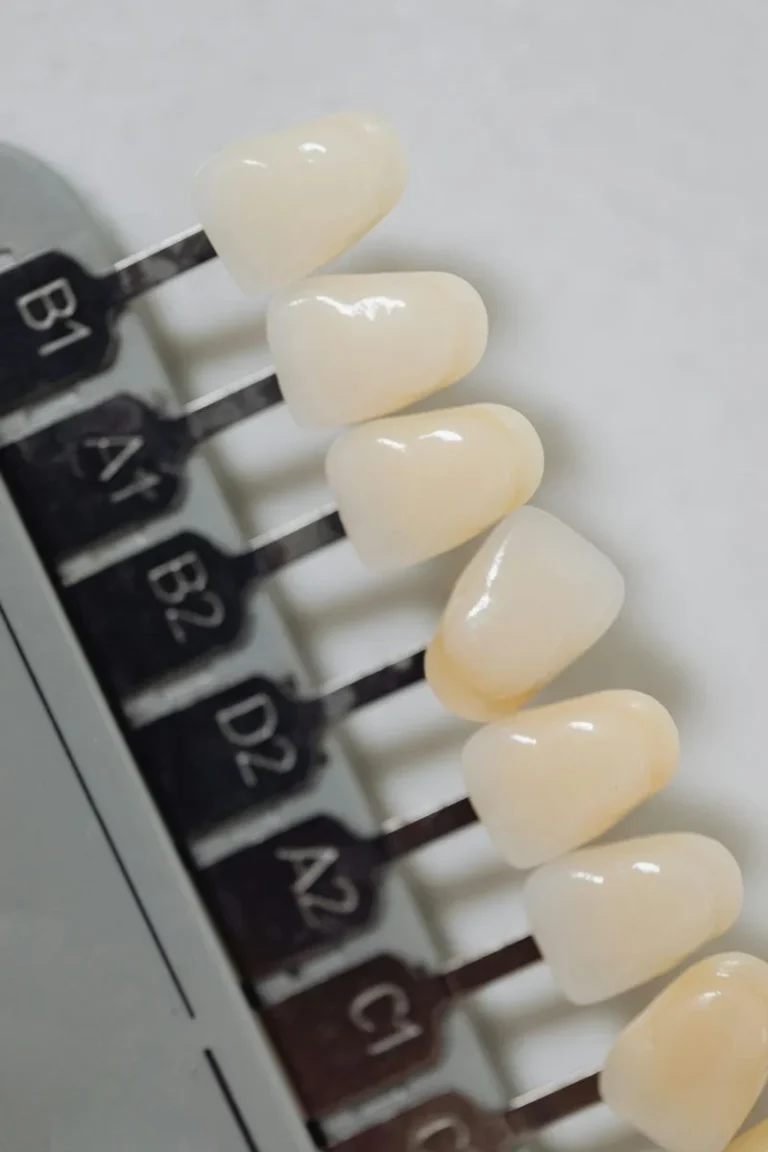
- If structural integrity is compromised due to long-term issues, restorative options like veneers might be needed, but preserving the natural foundation through collagen support is always preferred.
Conclusion: Collagen – The Connective Tissue Cornerstone of Oral Health
Collagen is far more than just a buzzword in skincare; it is the fundamental structural protein that underpins the health and resilience of our gums, anchors our teeth securely, and even contributes to the integrity of the teeth themselves. Its role in providing strength, enabling flexibility, facilitating healing, and forming a protective barrier is indispensable. Recognizing the factors that support healthy collagen – like adequate nutrition (especially Vitamin C), good oral hygiene, avoiding tobacco, and managing systemic health – empowers us to take proactive steps towards maintaining not just healthy gums and teeth, but overall oral wellness.
Don't Delay Your Treatment
Let's create your personalised treatment plan right away with a complimentary consultation with our specialist dentists.
By appreciating and supporting this vital protein network, we invest in the long-term stability, function, and health of our smiles.
Support Your Oral Foundation with Genç Dental
Understanding the importance of collagen is key to appreciating the foundations of a healthy mouth. At Genç Dental, we focus on comprehensive care that supports the health of all your oral tissues, including the vital collagen network within your gums, ligaments, and bone. Our experienced team emphasizes preventive strategies, early disease detection, and treatments designed to preserve and restore oral health effectively.
Whether you need routine check-ups, treatment for gum disease, advice on nutrition for oral health, or restorative procedures that rely on a healthy tissue foundation, we are here to provide expert, personalized care. Contact Genç Dental today to schedule your appointment and let us help you build and maintain the strong, collagen-supported foundation essential for a lifelong healthy smile.